In the fast-paced world of modern medicine, some culprits of serious disease hide in plain sight—quiet, unassuming, and often overlooked. One such biochemical troublemaker is homocysteine.
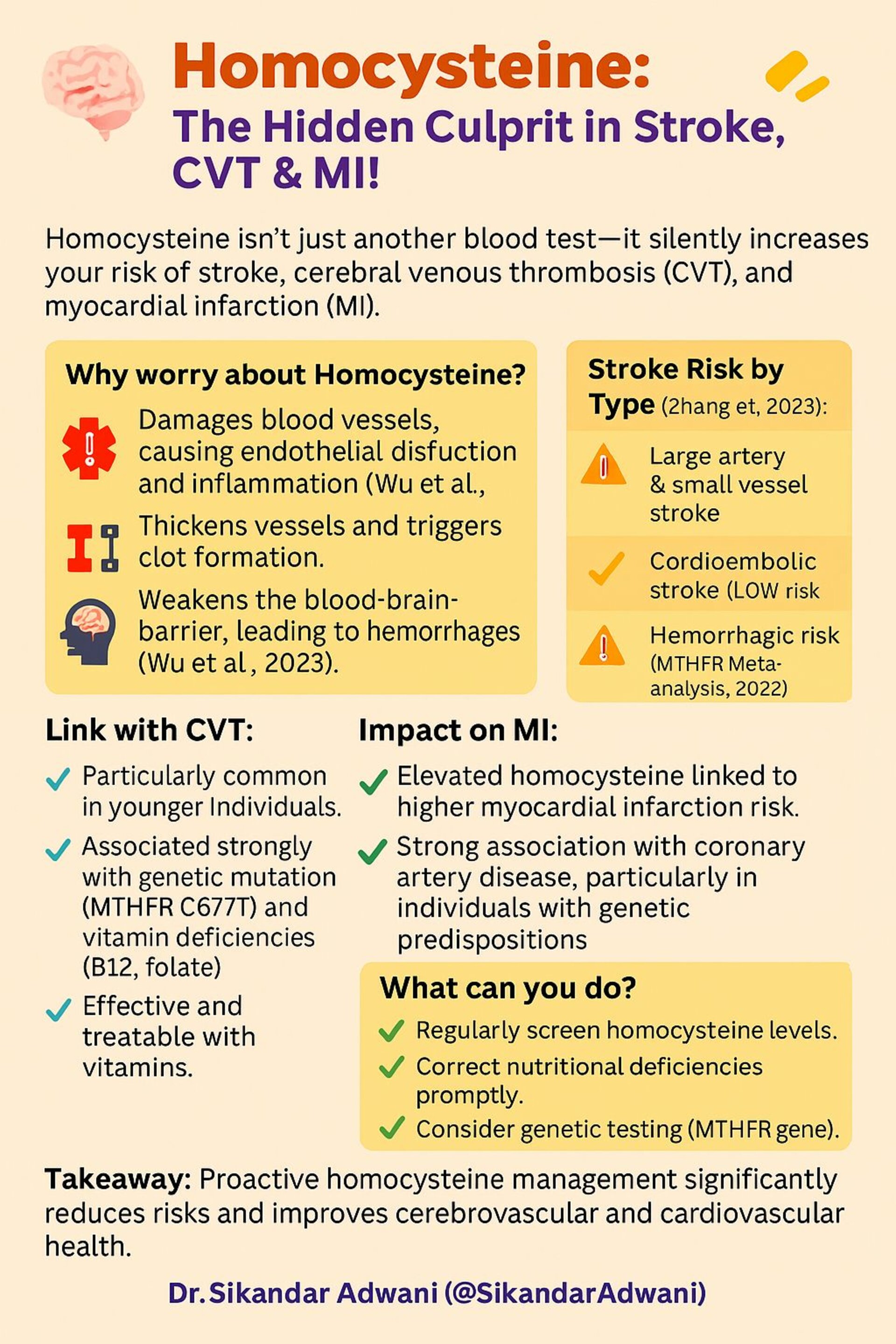
Often bundled away in a routine blood test, homocysteine is a sulfur-containing amino acid that, when elevated, can quietly damage your blood vessels and sharply raise your risk of stroke, cerebral venous thrombosis (CVT), and even myocardial infarction (MI). This blog will walk you through why homocysteine matters, who is at risk, and what you can do to protect yourself.
What Is Homocysteine and Why Should You Care?
Homocysteine is produced during the metabolism of methionine, an essential amino acid obtained from our diet. Under normal circumstances, your body converts homocysteine into other harmless substances with the help of folate, vitamin B6, and B12. But when this conversion process is impaired—due to genetic, nutritional, or lifestyle factors—homocysteine levels build up in the blood, causing a cascade of vascular problems.
Why it’s dangerous:
- It damages the endothelium, the delicate lining of blood vessels, leading to inflammation and dysfunction.
- It thickens arterial walls and promotes clot formation.
- It weakens the blood-brain barrier, raising the risk of hemorrhagic strokes.
Stroke, CVT, and MI: The Triple Threat
Stroke Risk and Homocysteine (Zhang et al., 2023)
Elevated homocysteine is strongly linked to:
- High risk of large-artery and small-vessel ischemic strokes
- Moderate risk of hemorrhagic stroke (MTHFR Meta-analysis, 2022)
- Low risk in cardioembolic stroke subtypes
CVT (Cerebral Venous Thrombosis)
- Particularly common in younger individuals
- Strongly associated with the MTHFR C677T gene mutation and deficiencies in vitamins B12 and folate
- Frequently underdiagnosed but easily treatable with proper supplementation
Myocardial Infarction (MI)
- Elevated homocysteine increases the risk of coronary artery disease and MI
- Strong links in individuals with genetic predispositions or poor nutritional status
The Clinical Consequences
High homocysteine isn’t just a risk factor on paper. It has real-world implications:
- Increases stroke severity
- Slows neurological recovery
- Raises the chances of hemorrhagic transformation after ischemic stroke
- Accelerates white matter degeneration on brain imaging
What the Latest Research Says
- CSPPT Trial (2015): Supplementing folic acid reduced stroke risk by 21% in hypertensive patients.
- Meta-analysis (2023): Confirmed a 10% reduction in stroke risk, especially in folate-deficient populations.
- VISP (2004) & VITATOPS (2010): Showed limited benefit in reducing recurrent stroke risk in folate-replete regions.
What Can You Do to Lower Your Risk?
- Screen regularly: Check your homocysteine levels during routine blood work, especially if you have a family history of stroke or heart disease.
- Correct nutritional deficiencies: Supplement with folate, vitamin B6, and B12 if needed.
- Get genetically tested: If you have unexplained vascular events or a family history, testing for *MTHFR C677T may be valuable.
- Lead a vascular-friendly lifestyle: Stop smoking, reduce alcohol, exercise, and manage other risk factors like blood pressure and cholesterol.
The Bottom Line
Homocysteine may not be as well-known as cholesterol or blood sugar, but its effects on your vascular system are just as serious. The good news? It’s modifiable. Through early detection, dietary correction, and lifestyle change, you can manage your homocysteine levels and reduce your risk of life-altering events like stroke, CVT, and MI.